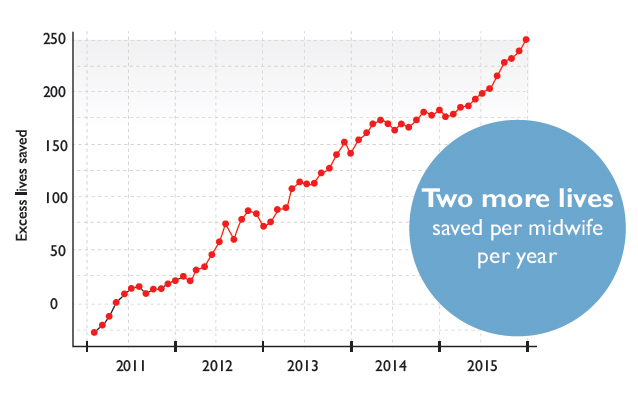
Helping save 500,000 more newborns a year by 2030 and preventing 50,000 more maternal deaths, account for more than half of the One Million Lives goal. Worldwide, nearly 3 million newborn deaths and 1.3 million fresh stillbirths occur each year, 99% of them in low- and middle-income countries (LMICs). This chapter relates to the needs and initiatives in LMICs, but the initiatives can also feed into making births in high-income countries safer.
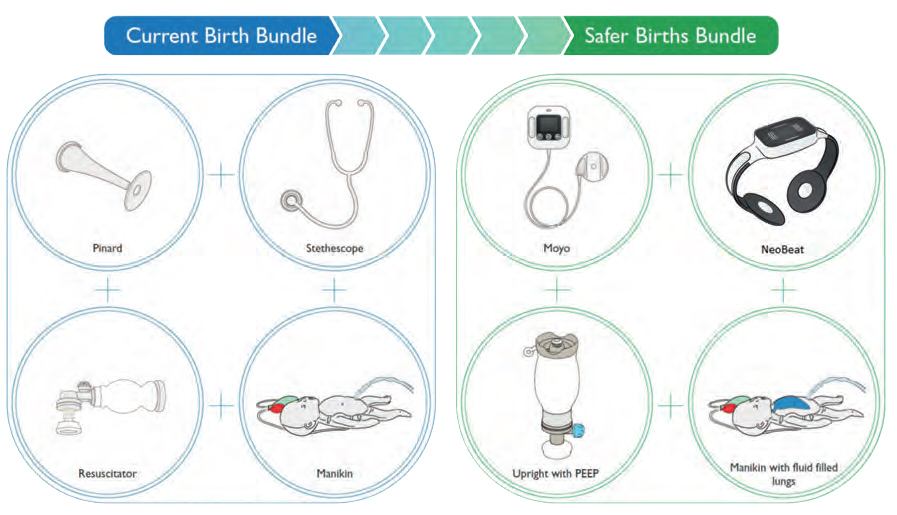
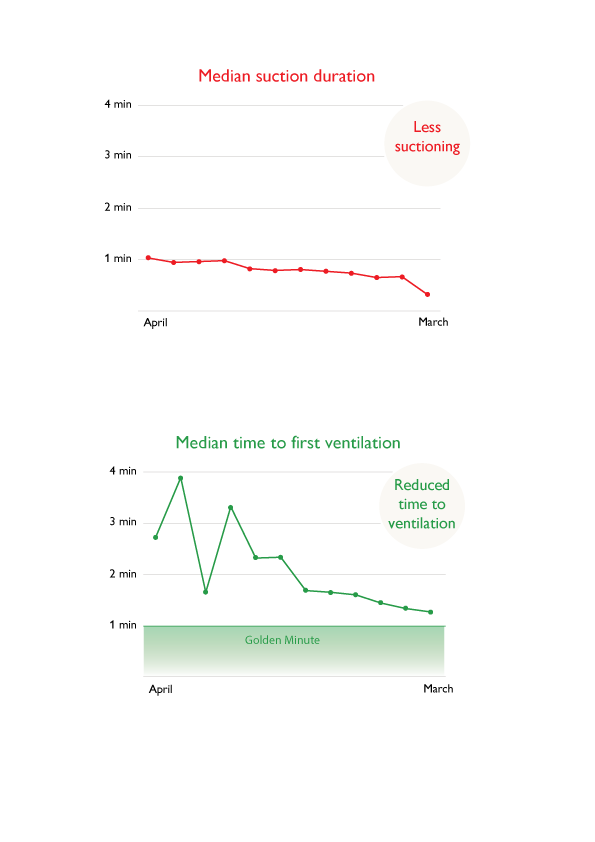
Birth-related complications cost about 200,000 maternal lives each year. In most of these cases simple procedures will suffice to save both mother and baby – if the birth attendant is well trained and confident. Early detection and treatment of complications greatly improve the chances of a good outcome.
SDG3 on health and well-being for all is more holistic than the previous health MDGs. With every life saved there is a significant amount of life years saved. Estimating that each saved baby will live for 70 years and each mother for 50, achieving the goal of saving 550,000 mothers and newborns means nearly 40 million life years gained – that is not counting the cases of prevented disablement.
As the shift progresses from donorship to ownership – the means of providing aid to enable governments and people to help themselves – partnerships are becoming increasingly important and are the bedrock of Laerdal’s approach to helping improve global health.